

Itchy feet, redness between the toes or even scaly skin on the heels – sound familiar? But watch out, because although foot fungus is one of the most common fungal diseases in industrialized countries, many people overlook the signs or do not know how to interpret them correctly. The treatment of athlete’s foot is promising – but only if you recognize it.
What causes athlete's foot?
In medical terminology, foot fungus is also called tinea pedis. This is a skin fungal disease that is mostly triggered by filamentous fungi. Less frequently, athlete’s foot is caused by other types of fungi such as yeast, sprouts or even molds.
When fungal spores hit the skin and penetrate the top layer of skin (callus), they can multiply there and cause an infection. However, the penetration of the fungi into the skin layer actually only succeeds when the protective mechanisms of the skin are weakened. Foot fungus therefore often develops when fungal spores enter the skin through small cracks or when the immune system, the acid mantle or the skin flora are weakened.
However, there are also certain risk factors that can promote the development of foot fungus. Damp feet in socks and shoes, often caused by synthetic materials, promotes a fungal infection, as this provides the perfect environment for fungi. In addition, age is also a risk factor – the risk of athlete’s foot increases with age. Other risk factors for foot fungus, are the following:

Detect athlete's foot and interpret symptoms correctly
The signs of foot fungus are usually rather inconspicuous at the beginning, such as itching between the toes, slightly reddish skin or perhaps already light skin flakes. However, the symptoms can intensify within a few days. The scaling is thus already after a few days significantly increased than in healthy feet. In advanced stages, white skin plates can also form, some of which look like calluses. If the foot fungus is not treated, this can also lead to the formation of painful cracks. Further, pain or burning sensation on the feet are also symptoms of foot fungus and should be closely monitored.
In advanced stages, blistering or sores that ooze are also common. Open or sore spots and burst blisters pose an additional risk. Pathogens and bacteria can penetrate and cause further inflammation of the foot. If bacteria colonize the affected areas, this can lead to an unpleasant odor that differs from normal foot odor. Unpleasant odor can thus be an indicator of foot fungus.

INFO: The symptoms of foot fungus do not always occur simultaneously, but can vary and differ in intensity. However, the symptoms often occur on both feet at the same time.
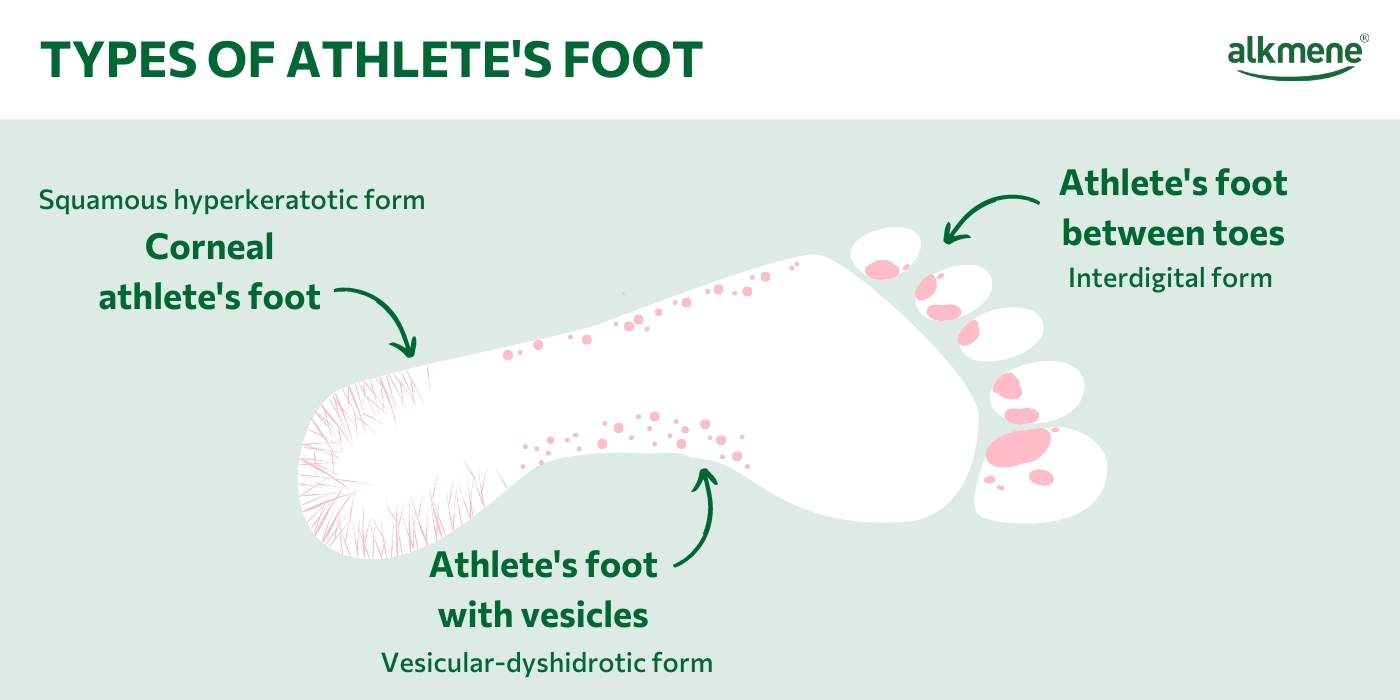
What are the different types of athlete's foot?
Not all athlete’s foot is the same! In medicine, a distinction is made between three different types of foot fungus:

IMPORTANT: If you experience these or similar symptoms, it is better to consult a doctor in order to recognize a possible athlete’s foot disease and to be able to treat it accordingly.
This form of athlete’s foot occurs between the toes. It is the most common type of athlete’s foot and accounts for about 80% of athlete’s foot infections. In the initial stage, the foot fungus occurs here in most cases between the 4th and 5th toe and then spreads to the further spaces between the toes. Symptoms here range from mild redness and scaling to thicker skin deposits, cracks or even blisters on the toes.
Squamous-hyperkeratotic foot fungus first affects the heels and balls of the feet and then spreads over the edges of the feet to the tops of the feet. Diabetics are particularly susceptible to this type of foot fungus. Typical symptoms here are scaly and very keratinized skin areas that are slightly inflamed at the beginning and then develop into painful tears in the foot.
This is a form of foot fungus that occurs primarily on the edge and arch of the foot. This type of foot fungus occurs most rarely. Common symptoms are blisters on the affected areas. Since there is often a thicker layer of cornea on the arch and edges of the foot, the blisters are less likely to burst here, but are more likely to dry out. This can lead to a feeling of tension and itching.
Is athlete's foot contagious?
All types of foot fungus are very contagious, as the falling skin scales contain fungal spores that can thus be transmitted to other people. These fungal spores can even survive for several days in the dead skin scales.
It is also important that not only other people can be infected, but also other body regions on the own body. If the foot fungus remains untreated for a longer period of time, it first spreads to the ankles. However, the infection can also spread to the nails and become nail fungus. If you scratch affected areas and then touch other parts of your body, such as your face, the foot fungus can be transmitted and spread there as well.
Athlete's foot treatment - How to get rid of foot fungus?
If the athlete’s foot is detected, it can be treated well and completely. This means that the infection disappears completely. However, it is important that the foot fungus is treated in time and consistently. If this does not happen, the disease can also become chronic.
For the treatment of foot fungus, antimycotics are used in the form of ointments or tablets to be taken. The antifungals work either by killing the fungi present or by inhibiting their multiplication. Since at the beginning of athlete’s foot treatment it is often not yet clear which fungal pathogen is the trigger for the infection, broad-spectrum antibiotics are often used here until a specific agent is switched.
During athlete’s foot treatment, there are also a few things to keep in mind:
After showering, it is important to dry the feet thoroughly before putting on socks or even shoes, so that the fungal pathogens are not offered the optimal moist environment.
For socks, the rule is to change them daily and wash them at a minimum of 60 degrees or, even better, 90 degrees. This is important to ensure that all pathogens are killed. In addition, a special hygiene detergent should be used here. Towels and bed linen should also be washed in this way and changed frequently.
The shoes worn should be sprayed with disinfectant spray during the athlete’s foot treatment, preferably daily, in order to kill possible fungal pathogens and spores here as well.








